Ectopic pregnancy
Under normal conditions, fertilization occurs in the tubal fimbria, the fertilized egg (zygote) remains in the tube for a few days, and is later implanted in the uterine cavity.
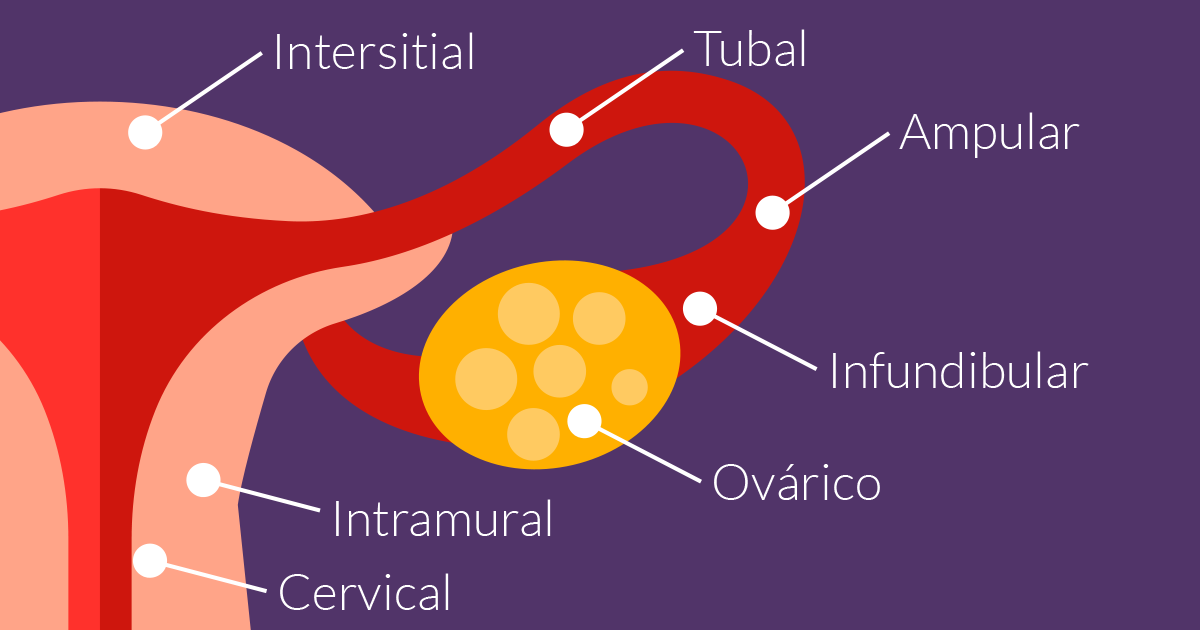
Ectopic pregnancy (EE), therefore, is the result of implantation of the zygote outside its usual place, which is the uterine cavity.
When they occur, 70% of these pregnancies are located in the uterine tube and the rest in other areas.
Frequency
In Mexico it occurs in approximately 4-6% of pregnancies in women between 15-44 years of age. However; in assisted reproduction treatments this figure can increase to 8%.
In our experience at Creafam, the presentation of ectopic pregnancy is close to 5-6%.
Present
In patients undergoing assisted reproduction treatments, the frequency may be slightly higher than in the general population, mainly due to factors such as: inflammatory tubal pathology, age, previous conservative surgeries, and a history of previous EE.
Fortunately, early diagnoses and clinical suspicion mean that this problem is resolved in the vast majority of cases without the need for surgical intervention, and initially conservative management is sufficient with the use of medications.
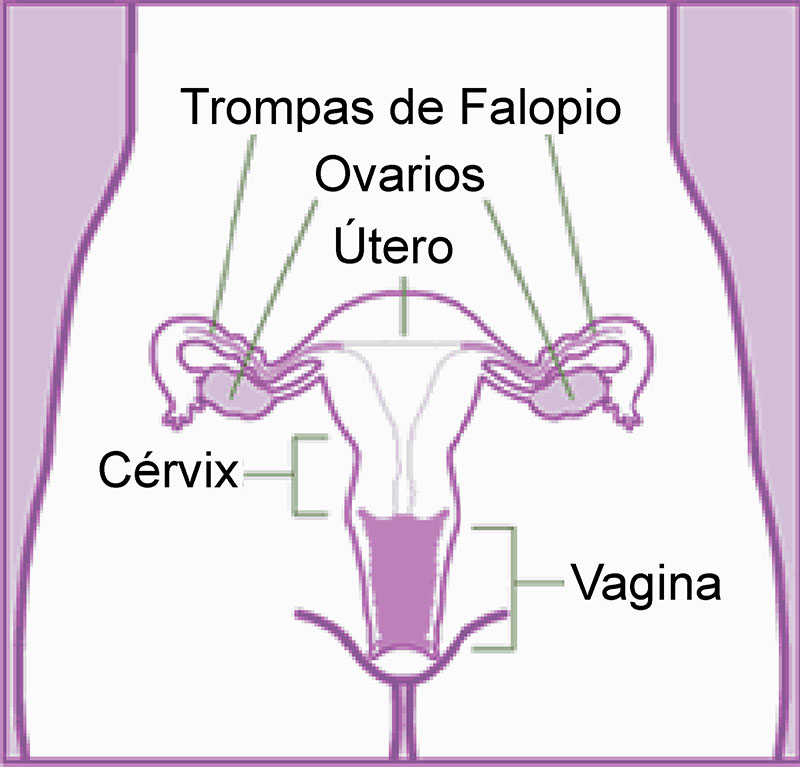
Anatomy
In the following figure we can see the anatomical structures of the female internal genitalia, which are located within the pelvic cavity, and their relationship to better understand where the most frequent site of presentation of EE is.
Diagnosis.
Although there is no pathognomonic symptom of EE (which appears only in the context of a disease), it is important to be aware of the combination of sudden abdominal pain, menstrual disturbances after a short absence of menstruation (amenorrhea), and previous symptoms of pregnancy. The most frequent symptoms are:
It is very important that the clinician suspect EE in order to be more thorough in his physical examination, with the following typical signs:
Analytics.
Whenever there is an implantation of the zygote in the uterine cavity and/or outside it, the Human Chorionic Gonadotropic Hormone in its beta (b) fraction (b-HCG).
In a normal pregnancy, the b-HCG fraction doubles its values every 2-3 days, in the EE this increase does not usually occur.
The use of vaginal ultrasound has come to improve and simplify early diagnosis, as well as its suspicion.
With a b-HCG greater than 1000 mIU/mL and an ultrasound without evidence of a gestational sac in the uterine cavity, it could be pathognomonic for EE.
Treatment.
There are 3 large groups of treatment that are:
It is of the utmost importance that when an EE is suspected, care with a specialist is not delayed, in the private sphere we hardly have maternal morbidity and mortality but it is still a problem that can lead to anything from an acute abdomen, hypovolemic shock until the death of the mother.